TS
rossdeleon
'Shell Shock'—The 100-Year Mystery May Now Be Solved
A research team in the United States may have solved a mystery that has haunted soldiers and veterans for more than a century: how blast force from battlefield explosions injures the human brain.
The findings, published Thursday in the medical journal the Lancet Neurology, reveal a unique and consistent pattern of damage in the autopsied brains of eight military service members who had served in Iraq, Afghanistan, and elsewhere in the Middle East.
All had suffered trauma after exposure to blast force on the battlefield, mostly from improvised explosive devices (IEDs)—the signature injury of recent campaigns, just as shell shock from exploding artillery shells had been the signature injury of World War I, a hundred years before.
In medical terminology, traumatic brain injury, or TBI, covers conditions that range from penetrating head wounds to blunt-force trauma typical of concussions.
But as the new study claims to demonstrate, the pattern of damage caused by exposure to blast force observed in the eight military personnel is distinct from that commonly observed in the brains of football players or boxers who have suffered blunt-force TBI.
Outside medical opinion has yet to weigh in on the findings. But Daniel Perl—a neuropathologist at the Uniformed Services University of the Health Sciences, in Bethesda, Maryland, who led the team behind the groundbreaking paper—said that when he realized that the lesion representing blast damage was distinctive, he knew it was the kind of once-in-a-lifetime breakthrough scientists dream of.
“What we found was a pattern of scarring that in 40 years of examining thousands of brains at autopsy I’ve never seen before and as far as I know is not described in any of the medical literature,” Perl said.
The implications of this finding are profound, pointing to the possibility that symptoms long thought to be psychological—ascribed to post-traumatic stress disorder (PTSD)—may instead be direct results of physical damage to the brain.
“It will mean reevaluating people we’ve labeled as having PTSD,” Perl said. “There’s nothing obvious in terms of treatment, but at least it suggests that one should not think about approaching the problem as a purely mental health problem.” It would mean reexamining such treatments as talk therapy and psychological medications.
The blast shock finding also opens up potentially fertile new ground for research: Can the injury be healed or even mitigated? What equipment can be designed to protect service members against blast damage to their brains? Can tests be devised to identify damage in combatants on the battlefield in real time?
And it raises a philosophical question for young men and women drawn to military service: If you know that exposure to a blast event—the signature mechanism of injury in modern warfare–may well irreparably damage your brain, will you still join up?
From the earliest years of the Iraq campaign, military personnel exposed to blast reported symptoms that included headache, sleeplessness, problems with memory and concentration, mood disorders such as anger and depression, and impulsiveness. Many of these symptoms are also characteristic of PTSD, which afflicts an estimated 11 to 20 percent of all veterans of the wars in Iraq and Afghanistan in any given year.
Medical practitioners therefore initially assumed the symptoms to be psychological. Furthermore, no routine imaging technology had succeeded in identifying any evidence of physical injury to the brain. But by the end of the first decade of this century, researchers had begun to recognize that while blast damage could not be seen, it was nonetheless real.
The U.S. Department of Defense estimates that some tens of thousands of U.S. veterans and military service members deployed in Iraq and Afghanistan have sustained traumatic brain injury as a result of exposure to a blast event. But given that exposures to blast events were not even logged in the early years of the campaigns, the figure may be much higher.
One of the brains that the team studied also showed signs of chronic traumatic encephalopathy (CTE), a neurodegenerative disease caused by the repetitive blunt-force trauma typical of concussions sustained in contact sports. Another showed features suggestive of an extremely early stage of the disease.
“CTE is not what these service members are suffering when they come home,” Perl said. “But this study suggests there are further concerns. They come home with the symptoms caused by the immediate damage—the blast injury—but down the line, in decades, many of these guys will also be hit with CTE.”
A wide array of research has attempted to discover the nature of blast injury. (See “The Invisible War on the Brain,” National Geographic, February 2015.) Efforts have included sophisticated studies of the physics of blast itself, as well as lab experiments conducted on animals, computer modeling of blast effects, and searches for biomarkers of blast exposure.
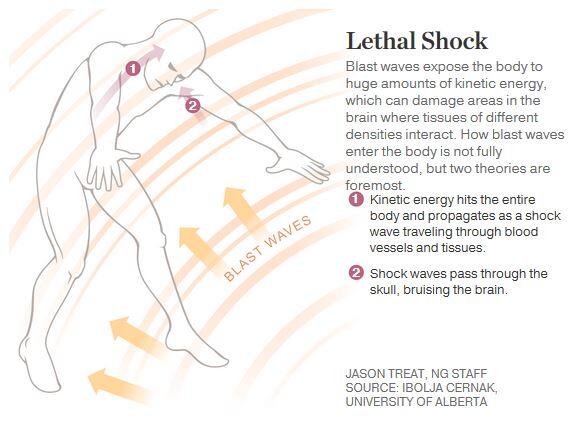
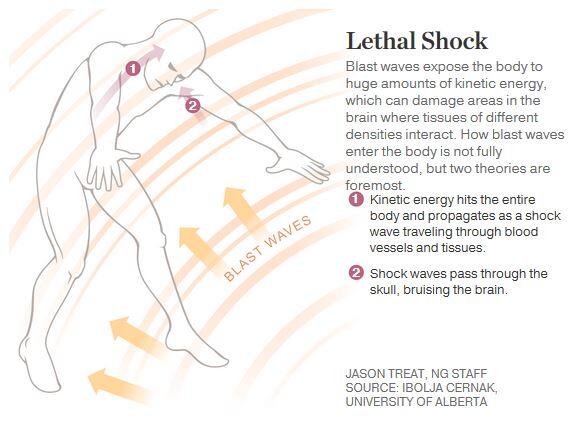
An explosion is a complex event that unleashes multiple mechanisms of injury. The primary blast effect is the shock wave, a balloon of rapidly expanding gases that compresses surrounding air and advances outward from the detonation faster than the speed of sound. This shock wave is what enters the brain, passing so rapidly that it has come and gone before the people hit have even had time to move their heads.
Just how a shock wave enters the brain is still not understood. Some believe entry is through the natural openings in the skull: the eye sockets, ears, nostrils, and mouth. Another theory is that since shock wave pressure hits the entire body, not just the head, it’s transmitted into the chest or abdominal cavities and surges to the brain by way of the body’s vasculature.
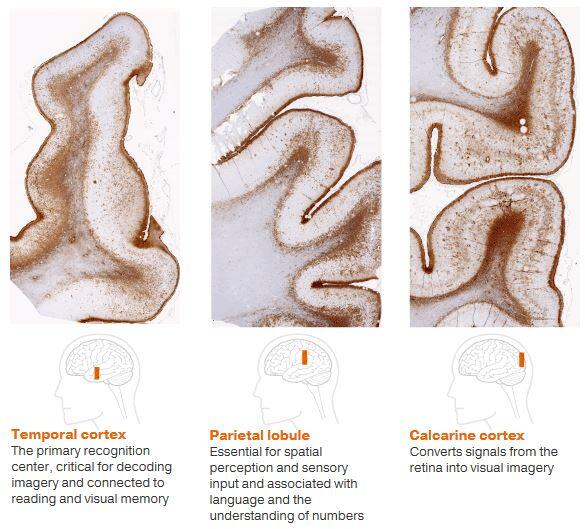
Once inside the skull, the wave advances through the brain at the speed of sound, passing through both fluids and matter, which respond differently to the wave’s properties. As the new paper reports, the distinctive pattern of scarring occurs precisely in those places where different compositions of brain tissue intersect.
In 2013 the Department of Defense established the Center for Neuroscience and Regenerative Medicine Brain Tissue Repository, under the direction of Perl, to pursue postmortem study of brains at the tissue level.
“Our microscopes have resolutions a thousand times greater than any imaging technology,” Perl said. “Autopsy is the gold standard for this kind of investigation.”
The eight brain specimens his team studied represented chronic cases, in which the person had lived at least six months after the blast event, as well as acute cases, in which death had followed within 60 days. “The acute cases are revealing,” Perl said. “The injury is only four days old, and yet we see the very beginning of the foundation of scars. And these early signs—these early scars—are in the right places, form the right pattern.”
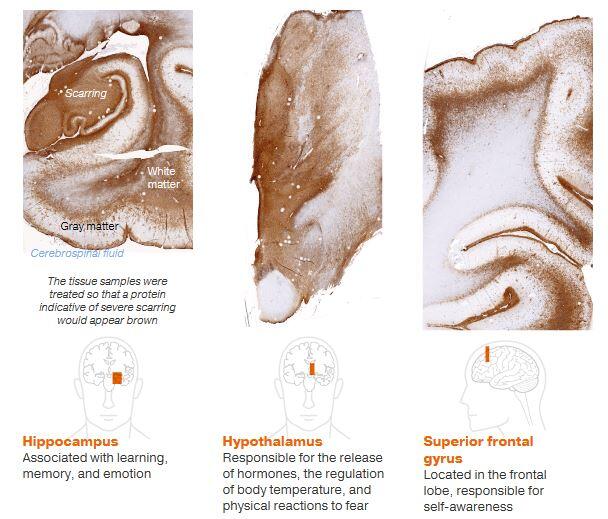
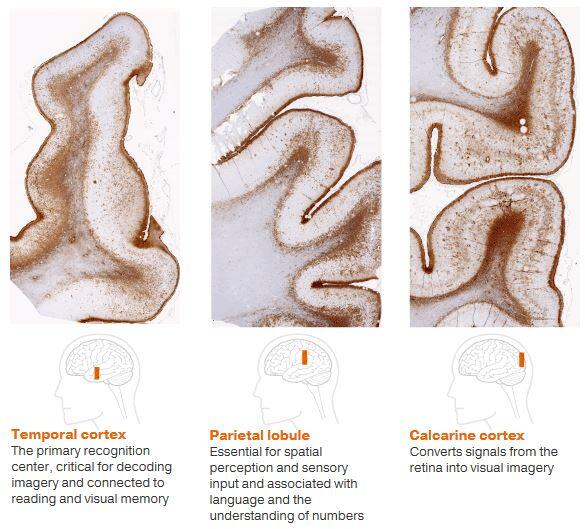
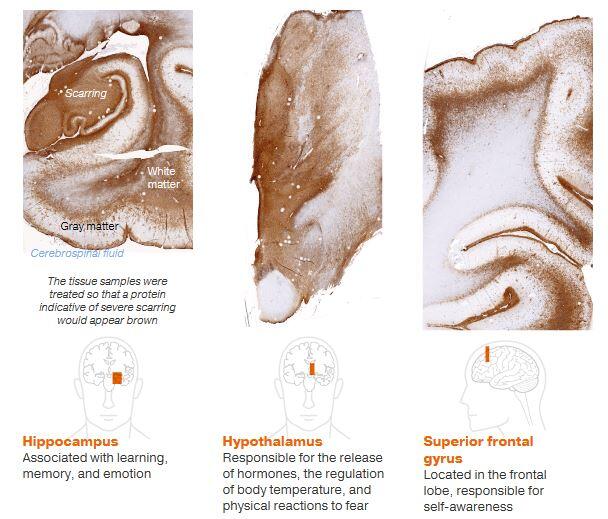
Blast waves seem to cause damage at the boundaries of different structures, such as between brain matter and cerebrospinal fluids and between gray and white brain matter. That damage, Perl said, “is consistent with experiments that have modeled blast waves’ effects on the different substances forming the brain.”
More starkly revealing than any words are the brain images that illustrate what Perl describes. Panels show brain tissue, as delicate as butterfly wings, spatter-marked as if with buckshot, bearing outright tears surrounded by broken tendrils of scarring or dark clouds of damage looming from the folds and furrows.
This blast damage reaches its spider legs into different regions of the brain: the frontal lobe, which controls attention span and emotional control; the hypothalamus, which regulates sleep; the hippocampus, responsible for the formation of memories. The symptoms resulting from damage to these areas are exactly the kinds of symptoms often attributed to PTSD.
What the Eight Men Endured
Emerging from the welter of medical data are details about the lives of the men who make up the research study. They had all been exposed to bombs, IEDs, and high explosives, and they had lived from as long as nine years after blast exposure to as little as four days. They ranged in age from 26 to 45 at the time of death. They had endured headaches, anxiety, depression, insomnia, memory and concentration problems, seizures, and chronic pain.
One was a Navy SEAL who conducted explosives training exercises and lost his coherence of thought; he began to jumble his speech and became overwhelmed by such routine tasks as driving or even packing a car.
Three of the men had acute brain injury and died shortly after exposure to the explosion, suffering burns, fractures, and hemorrhage. Four of the remaining five men who had chronic blast-induced brain injury died by suicide or from drug overdoses. The cause of death of the eighth service member was not determined.
In December 2015, Congress passed a bill mandating the Department of Defense and the Department of Veterans Affairs to examine the effects of combat service “on suicides and other mental health issues among veterans.”
The new paper may add to mounting evidence that destructive behaviors, including suicide, are outcomes directed by damaged regions of the brain—as symptomatic of blast damage as such common conditions as sleeplessness and ringing in the ears.
Déjà Vu
A century ago, in February 1915, the Lancet, the parent journal of the Lancet Neurology, published the first medical case study of shell shock in World War I. In the war’s aftermath, medical judgment held that thousands upon thousands of shell-shocked men were “neurasthenic” or subject to “neuroses.”
These mostly young veterans suffered through their lives in the belief that they had lost their nerve on the field of battle—in short, that they had failed. From the British government Ministry of Pensions files we can catch occasional glimpses of their postwar fates.
One case: a shell-shocked soldier who’d spent 118 days in the hospital being treated for loss of speech, inability to sleep, and loss of memory and concentration—and had been returned to active duty. Case notes made after the war remark on his complaints about “general weakness” and tremors in his hands. It is noted that his mental development is poor, and his answers to questions are “vague and contradictory.” Then, like so many others, he slips from history’s sight.
“We can’t let this happen again,” Daniel Perl said. “This study will certainly stimulate important further research and, we predict, will dramatically change how we think about these problems.”
Beyond the specifically medical questions, the finding raises a number of issues, such as care costs many years into the future and whether those diagnosed with TBI should be awarded the Purple Heart.
“People that have seen the paper are very excited about it. Blast people working on military TBI are very excited,” Perl said. “Then they start asking questions: How large a dose of blast is damaging? Are multiple small exposures doing this? How common is this?—I have a feeling this is pretty common. Can you see it by imaging? And so far the answer to all of these is, we don’t know.”
sumber : http://news.nationalgeographic.com/2...world-war-one/
The findings, published Thursday in the medical journal the Lancet Neurology, reveal a unique and consistent pattern of damage in the autopsied brains of eight military service members who had served in Iraq, Afghanistan, and elsewhere in the Middle East.
All had suffered trauma after exposure to blast force on the battlefield, mostly from improvised explosive devices (IEDs)—the signature injury of recent campaigns, just as shell shock from exploding artillery shells had been the signature injury of World War I, a hundred years before.
In medical terminology, traumatic brain injury, or TBI, covers conditions that range from penetrating head wounds to blunt-force trauma typical of concussions.
But as the new study claims to demonstrate, the pattern of damage caused by exposure to blast force observed in the eight military personnel is distinct from that commonly observed in the brains of football players or boxers who have suffered blunt-force TBI.
Outside medical opinion has yet to weigh in on the findings. But Daniel Perl—a neuropathologist at the Uniformed Services University of the Health Sciences, in Bethesda, Maryland, who led the team behind the groundbreaking paper—said that when he realized that the lesion representing blast damage was distinctive, he knew it was the kind of once-in-a-lifetime breakthrough scientists dream of.
“What we found was a pattern of scarring that in 40 years of examining thousands of brains at autopsy I’ve never seen before and as far as I know is not described in any of the medical literature,” Perl said.
The implications of this finding are profound, pointing to the possibility that symptoms long thought to be psychological—ascribed to post-traumatic stress disorder (PTSD)—may instead be direct results of physical damage to the brain.
“It will mean reevaluating people we’ve labeled as having PTSD,” Perl said. “There’s nothing obvious in terms of treatment, but at least it suggests that one should not think about approaching the problem as a purely mental health problem.” It would mean reexamining such treatments as talk therapy and psychological medications.
The blast shock finding also opens up potentially fertile new ground for research: Can the injury be healed or even mitigated? What equipment can be designed to protect service members against blast damage to their brains? Can tests be devised to identify damage in combatants on the battlefield in real time?
And it raises a philosophical question for young men and women drawn to military service: If you know that exposure to a blast event—the signature mechanism of injury in modern warfare–may well irreparably damage your brain, will you still join up?
From the earliest years of the Iraq campaign, military personnel exposed to blast reported symptoms that included headache, sleeplessness, problems with memory and concentration, mood disorders such as anger and depression, and impulsiveness. Many of these symptoms are also characteristic of PTSD, which afflicts an estimated 11 to 20 percent of all veterans of the wars in Iraq and Afghanistan in any given year.
Medical practitioners therefore initially assumed the symptoms to be psychological. Furthermore, no routine imaging technology had succeeded in identifying any evidence of physical injury to the brain. But by the end of the first decade of this century, researchers had begun to recognize that while blast damage could not be seen, it was nonetheless real.
The U.S. Department of Defense estimates that some tens of thousands of U.S. veterans and military service members deployed in Iraq and Afghanistan have sustained traumatic brain injury as a result of exposure to a blast event. But given that exposures to blast events were not even logged in the early years of the campaigns, the figure may be much higher.
One of the brains that the team studied also showed signs of chronic traumatic encephalopathy (CTE), a neurodegenerative disease caused by the repetitive blunt-force trauma typical of concussions sustained in contact sports. Another showed features suggestive of an extremely early stage of the disease.
“CTE is not what these service members are suffering when they come home,” Perl said. “But this study suggests there are further concerns. They come home with the symptoms caused by the immediate damage—the blast injury—but down the line, in decades, many of these guys will also be hit with CTE.”
A wide array of research has attempted to discover the nature of blast injury. (See “The Invisible War on the Brain,” National Geographic, February 2015.) Efforts have included sophisticated studies of the physics of blast itself, as well as lab experiments conducted on animals, computer modeling of blast effects, and searches for biomarkers of blast exposure.
An explosion is a complex event that unleashes multiple mechanisms of injury. The primary blast effect is the shock wave, a balloon of rapidly expanding gases that compresses surrounding air and advances outward from the detonation faster than the speed of sound. This shock wave is what enters the brain, passing so rapidly that it has come and gone before the people hit have even had time to move their heads.
Just how a shock wave enters the brain is still not understood. Some believe entry is through the natural openings in the skull: the eye sockets, ears, nostrils, and mouth. Another theory is that since shock wave pressure hits the entire body, not just the head, it’s transmitted into the chest or abdominal cavities and surges to the brain by way of the body’s vasculature.
Once inside the skull, the wave advances through the brain at the speed of sound, passing through both fluids and matter, which respond differently to the wave’s properties. As the new paper reports, the distinctive pattern of scarring occurs precisely in those places where different compositions of brain tissue intersect.
In 2013 the Department of Defense established the Center for Neuroscience and Regenerative Medicine Brain Tissue Repository, under the direction of Perl, to pursue postmortem study of brains at the tissue level.
“Our microscopes have resolutions a thousand times greater than any imaging technology,” Perl said. “Autopsy is the gold standard for this kind of investigation.”
The eight brain specimens his team studied represented chronic cases, in which the person had lived at least six months after the blast event, as well as acute cases, in which death had followed within 60 days. “The acute cases are revealing,” Perl said. “The injury is only four days old, and yet we see the very beginning of the foundation of scars. And these early signs—these early scars—are in the right places, form the right pattern.”
Blast waves seem to cause damage at the boundaries of different structures, such as between brain matter and cerebrospinal fluids and between gray and white brain matter. That damage, Perl said, “is consistent with experiments that have modeled blast waves’ effects on the different substances forming the brain.”
More starkly revealing than any words are the brain images that illustrate what Perl describes. Panels show brain tissue, as delicate as butterfly wings, spatter-marked as if with buckshot, bearing outright tears surrounded by broken tendrils of scarring or dark clouds of damage looming from the folds and furrows.
This blast damage reaches its spider legs into different regions of the brain: the frontal lobe, which controls attention span and emotional control; the hypothalamus, which regulates sleep; the hippocampus, responsible for the formation of memories. The symptoms resulting from damage to these areas are exactly the kinds of symptoms often attributed to PTSD.
What the Eight Men Endured
Emerging from the welter of medical data are details about the lives of the men who make up the research study. They had all been exposed to bombs, IEDs, and high explosives, and they had lived from as long as nine years after blast exposure to as little as four days. They ranged in age from 26 to 45 at the time of death. They had endured headaches, anxiety, depression, insomnia, memory and concentration problems, seizures, and chronic pain.
One was a Navy SEAL who conducted explosives training exercises and lost his coherence of thought; he began to jumble his speech and became overwhelmed by such routine tasks as driving or even packing a car.
Three of the men had acute brain injury and died shortly after exposure to the explosion, suffering burns, fractures, and hemorrhage. Four of the remaining five men who had chronic blast-induced brain injury died by suicide or from drug overdoses. The cause of death of the eighth service member was not determined.
In December 2015, Congress passed a bill mandating the Department of Defense and the Department of Veterans Affairs to examine the effects of combat service “on suicides and other mental health issues among veterans.”
The new paper may add to mounting evidence that destructive behaviors, including suicide, are outcomes directed by damaged regions of the brain—as symptomatic of blast damage as such common conditions as sleeplessness and ringing in the ears.
Déjà Vu
A century ago, in February 1915, the Lancet, the parent journal of the Lancet Neurology, published the first medical case study of shell shock in World War I. In the war’s aftermath, medical judgment held that thousands upon thousands of shell-shocked men were “neurasthenic” or subject to “neuroses.”
These mostly young veterans suffered through their lives in the belief that they had lost their nerve on the field of battle—in short, that they had failed. From the British government Ministry of Pensions files we can catch occasional glimpses of their postwar fates.
One case: a shell-shocked soldier who’d spent 118 days in the hospital being treated for loss of speech, inability to sleep, and loss of memory and concentration—and had been returned to active duty. Case notes made after the war remark on his complaints about “general weakness” and tremors in his hands. It is noted that his mental development is poor, and his answers to questions are “vague and contradictory.” Then, like so many others, he slips from history’s sight.
“We can’t let this happen again,” Daniel Perl said. “This study will certainly stimulate important further research and, we predict, will dramatically change how we think about these problems.”
Beyond the specifically medical questions, the finding raises a number of issues, such as care costs many years into the future and whether those diagnosed with TBI should be awarded the Purple Heart.
“People that have seen the paper are very excited about it. Blast people working on military TBI are very excited,” Perl said. “Then they start asking questions: How large a dose of blast is damaging? Are multiple small exposures doing this? How common is this?—I have a feeling this is pretty common. Can you see it by imaging? And so far the answer to all of these is, we don’t know.”
sumber : http://news.nationalgeographic.com/2...world-war-one/
Diubah oleh stuka1788 15-06-2016 00:53
0
5.9K
28
Thread Digembok
Urutan
Terbaru
Terlama
Thread Digembok
Komunitas Pilihan